Day 10: The problem with sleep medications
“So then I took an Ambien, and somehow I woke up on the roof…”
Yesterday, we started to discuss basic cognitive therapy skills. Today, we’ll address the facts behind one of the most common automatic negative thoughts: “I can’t sleep without a medication.” You may be taking a medication now, or you may have avoided them for any number of reasons. Let’s talk about why sleep medications are so common, and some important facts you might consider when deciding what to do about sleep medications.
Why doctors prescribe so many sleep medications
If you had to identify the worst possible place to sleep, you probably couldn’t imagine much worse than a hospital. Patients lie on uncomfortable beds and can’t escape from the lights in the hallway. They are surrounded by beeping machines, snoring roommates, and unpleasant smells. And to make matters worse, the sickest patients are typically woken up several times during the night for vital sign checks or blood draws. Since this environment is where essentially every physician begins their training, doctors become exceptional at prescribing medications that can help people sleep through anything.
In fact, many don’t even know that there is an effective alternative to medications. I had to go out of my way to learn about cognitive behavioral therapy for insomnia (CBT-I), and most of the medical students I’ve taught didn’t know about it either. I’m optimistic that this will improve as CBT-I becomes more well known.
Now, I’m not going to say that sleep medications are necessarily a bad thing. That would be disingenuous. In the right circumstances, a sleep medication can be a useful tool. But make sure you do your homework. Here are four things you should consider:
Fact 1: Scientific consensus strongly recommends CBT-I as the first-line treatment for insomnia.* Almost every study performed to date suggests that CBT-I matches or outperforms sleep medication treatment for insomnia. In addition, the benefits of CBT-I extend long after treatment stops, while the effects of medication treatments typically wear off when you stop taking your medication. For these reasons, CBT-I is considered the gold-standard intervention for insomnia.
CBT-I has been shown to work well when completed through self-help guides or over the internet. However, some people do better with personal support. If the CBT-I techniques you learn during Slumber Camp aren’t quite enough, I strongly recommend that you get in touch with a behavioral sleep specialist who can further troubleshoot your sleep through in-person CBT-I. If that doesn’t help, talking with your doctor about sleep medications and alternative diagnoses is a really good idea.
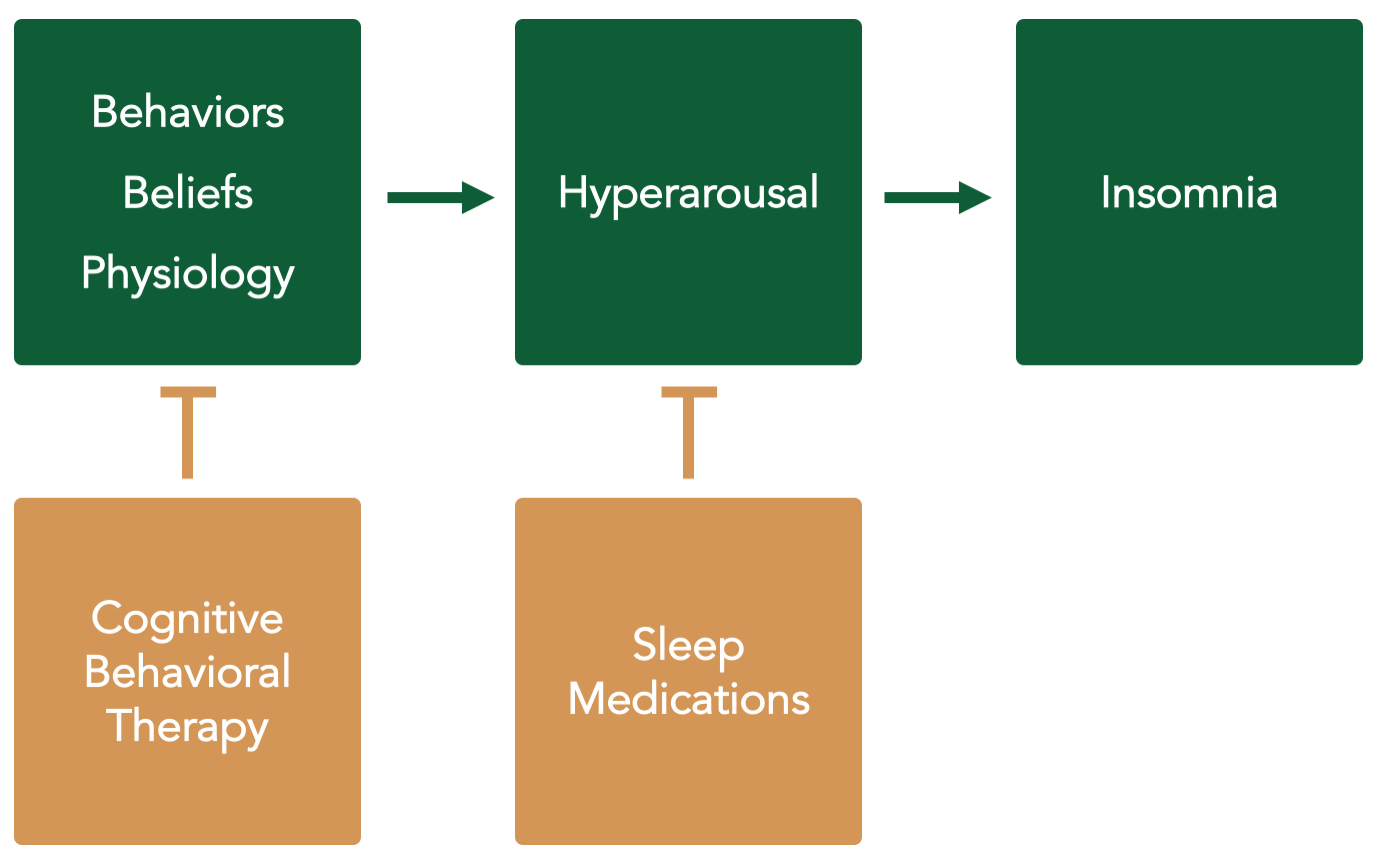
Fact 2: Sleep medications do not address the underlying cause of hyperarousal. Whenever possible, the goal of any treatment should be to address the root cause of a problem. As you now know, insomnia is caused by changes in behaviors, beliefs, and physiology that lead to persistent hyperarousal. CBT-I works because it addresses these factors. This can create lifelong improvements in sleep after just a few weeks of effort.
In contrast, sleep medications are designed to temporarily modify your sleep drive and wakefulness systems. They do this remarkably well over the short term, but they do not address the reversible contributions of behavior, beliefs, and conditioned arousal. Unless something changes in your underlying behaviors, beliefs, and physiology, chronic insomnia tends to stay in remission only if you keep taking medications.
Fact 3: All treatments have side effects. One of the first principles of pharmacology can be summarized as “anything powerful enough to help you is powerful enough to hurt you.” This means that all effective treatments have side effects, regardless of whether the treatment is medical, surgical, behavioral, nutritional, or natural. Balancing benefits and risks is an essential component of every treatment decision.
Every sleeping pill carries a risk of significant side effects, and your doctor is an excellent source for advice on this matter. In general, doctors worry when sleep medications cause excessive sedation, slowed breathing, falls, confusion, and addiction. These side effects—and their consequences—can be especially pronounced in older adults.
In addition, many people on sleep medications report better sleep, but they may not experience less sleepiness during the day because they still have medicine in their system. This “hangover effect” can be minimized with short-acting medications. However, these medications aren’t as helpful in people who have trouble getting back to sleep during the night.
Finally, all sleep medications change the natural cycle of your sleep, which may result in unforeseen changes to your level of sleepiness, fatigue, or memory formation.
CBT-I isn’t risk free either. However, surveys suggest that people report fewer side effects from CBT-I compared to medications. I suspect that you’ll have increased sleepiness and slower reaction time during the early phases of sleep restriction. This tends to rapidly improve as your sleep returns to a more normal cycle, but you must continue to be very careful if you choose to drive while engaging in Slumber Camp.
Fact 4: Sleep medications are not designed to be used every night. Every sleeping pill can lose some of its effectiveness when used over a long period of time. This phenomenon is called tolerance. Some sleep medications are associated with rapid tolerance. For example, the antihistamines diphenhydramine (Benadryl, ZzzQuil), doxylamine (Unisom, NyQuil), and hydroxyzine (Vistaril, Atarax) can lose some of their sleep-inducing abilities within a few days. Tolerance may develop more slowly with other medications, but it’s incredibly common in people who use a medication to sleep every night.
Long-term sleep medication use can also cause physical dependence. This does not mean that you are addicted to the medication. It simply means that your body will not respond well if you abruptly decrease your dose or stop taking it. Most people experience temporary sleep disturbances when they reduce their dose, a phenomenon called rebound insomnia. However, abrupt discontinuation of some medications can also result in seizures, delirium, and even death. This is especially true of the short-acting benzodiazepines such as alprazolam (Xanax), lorazepam (Ativan), and temazepam (Restoril). For these reasons, I strongly recommend that you work with your doctor before making changes to any sleep medications.
Even with all these facts in mind, it can be incredibly anxiety provoking to think about a life without sleep medications. Don’t worry about that too much today. On Day 27, we’ll talk through a practical plan for decreasing your medications. In the best case scenario, I often encourage people to keep a few tablets around for emergencies. When that’s not possible, the goal should be to balance medication use with quality of life.
For now, let’s keep pushing forward with CBT-I principles. Tomorrow, we’ll talk about how to manage worries so that you can more comfortably fall asleep.
Jeff Clark, MD
Camp Chemist
| Today’s Action List: | |
 |
Fill in your sleep log. Last night was Night 10. |
 |
Continue sleep restriction. (Wake up at the same scheduled time each day. Do not get into bed before your bedtime.) |
 |
Continue stimulus control. (Your bed is only for sleep and sex. Don’t go to bed unless sleepy. Get out of bed if you don’t fall asleep within 20 minutes.) |
| Recommended: | |
 |
Practice box breathing for 5 minutes. |
| Optional: | |
 |
Identify and reframe an automatic negative thought for Day 10. |
Tomorrow’s Lesson:
Stop worrying and start sleeping
Nerdy Footnotes:
* Check out these papers from the American Academy for Sleep Medicine, the American College of Physicians, and the European Sleep Research Society.
Copyright 2017 – , Wonderberry LLC (dba Slumber Camp). Fox image used under Creative Commons.