Information for Clinicians
Table of Contents
What is Slumber Camp?
What is CBT-I?
Myths about CBT-I
Is online CBT-I an evidence-based intervention?
Which insomnia subtypes respond to CBT-I?
Contraindications
Sleep medications and CBT-I
Price and Scholarships
Who are you and what do you think you’re doing?
Create a free clinician account
What is Slumber Camp?
Slumber Camp is an award-winning, 28-day, online course that teaches the principles of cognitive behavioral therapy for insomnia (CBT-I). CBT-I is recommended as the first-line treatment for insomnia by the American College of Physicians and the American Academy of Sleep Medicine.
What is CBT-I?
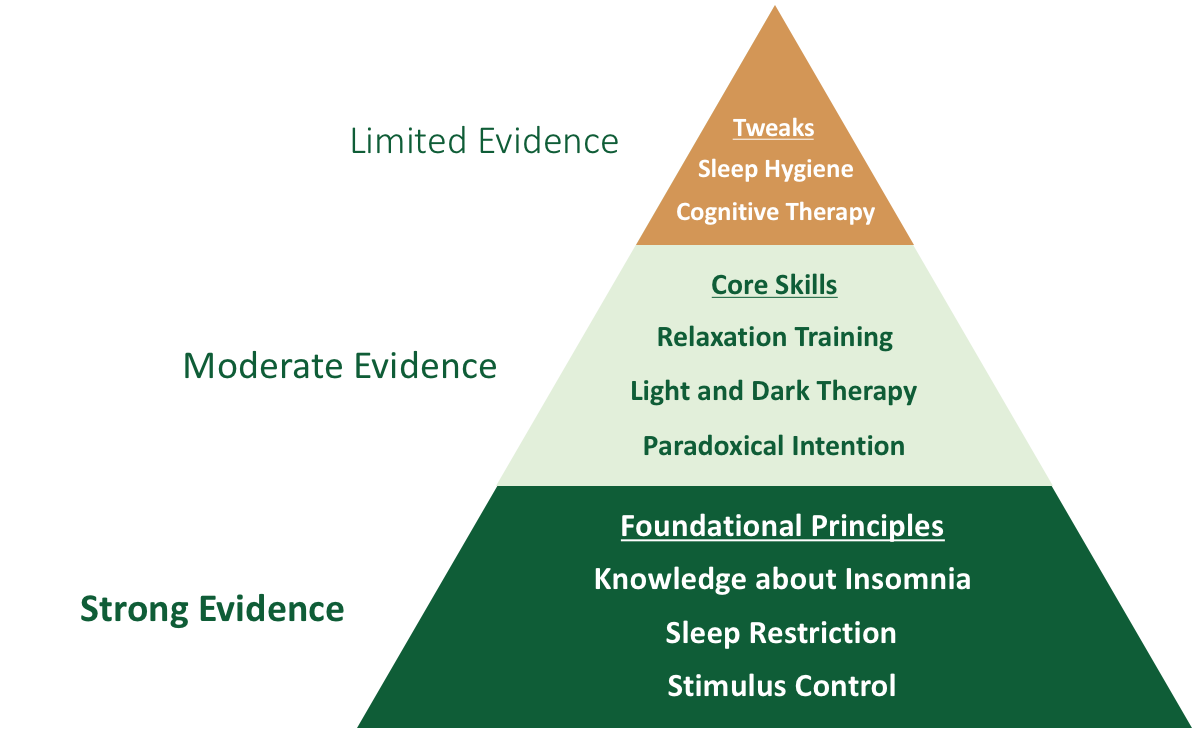
CBT-I is a behavioral treatment that asks participants to make counterintuitive changes to their sleep patterns. The foundational principles of CBT-I are called sleep restriction and stimulus control. These techniques have been shown to have a dramatic impact even when taught in one or two sessions with a primary care physician or mental health nurse practitioner.
Sleep restriction is a systematic protocol that asks participants to monitor their nightly sleep patterns, consolidate all of their time in bed into a single rest period, and then make weekly adjustments to optimize sleep efficiency. This requires a small amount of math which is usually done in session with a therapist. Slumber Camp uses a sleep calculator to automate this process.
Stimulus control is the extreme, literal interpretation of the sleep hygiene recommendation to “only use your bed for sleep and sex.” The goal is to break the association between the bed and wakefulness. During stimulus control, participants are asked to leave the bedroom if they have been awake for more than 20 minutes, engage in calm activities, and then only return to bed when they feel sleepy again. This technique is marginally effective when done casually, but incredibly potent when engaged in a rigorous, systematic way.
The remainder of CBT-I is focused on techniques which have more modest evidence and effect sizes. In Slumber Camp, we call techniques with significant evidence core skills. These include relaxation training, light and dark management, and paradoxical intention. In addition, we discuss ideas which have theoretical value, but limited evidence in the treatment of insomnia. I call these principles tweaks, and they include sleep hygiene education and traditional cognitive therapy techniques. Slumber Camp focuses heavily on the foundational skills of sleep restriction and stimulus control, and then adds in core skills and tweaks as participants progress through the course.
Myths about CBT-I
CBT-I is sleep hygiene. This is false. Sleep hygiene may be included in CBT-I interventions, but there is little evidence that sleep hygiene education is an effective intervention for insomnia, either as monotherapy or when added as a component of CBT-I. In Slumber Camp, I deliberately de-emphasize these principles until strong, evidence-based behavioral patterns have been established. Sleep hygiene principles are treated as tweaks—theoretically useful skills that can be applied if they seem helpful to the participant.
CBT-I is a cognitive treatment focused on changing thinking patterns. This is false. CBT-I is primarily a behavioral treatment that focuses on altering maladaptive bedroom behavior. Cognition often changes through experiential learning, but this is a secondary effect. If you have some familiarity with CBT, you will know about a technique known as cognitive restructuring, which has been widely popularized in books like Feeling Good. This technique may be helpful in the treatment of depression and anxiety, but there is little evidence that traditional cognitive therapy interventions improve insomnia symptoms. In other words, other forms of CBT won’t address the core components of CBT-I that people with insomnia need to recover. For these reasons, Slumber Camp treats cognitive therapy as a tweak.
CBT-I focuses heavily on mindfulness meditation. This is mostly false. The earliest forms of CBT-I used progressive muscle relaxation, and some practitioners now use mindfulness meditation as one component of the therapy. There is reasonable evidence to support the addition of a relaxation training component to sleep restriction and stimulus control. During Slumber Camp, participants are taught deep breathing, mindfulness meditation, and progressive muscle relaxation after starting sleep restriction and stimulus control. Each of these three skills is practiced for a full week, so that participants have a chance to discover a technique they find useful. As relaxation training does have significant evidence, it (along with light and dark management and paradoxical intention) is considered a core skill.
CBT-I is only effective in people with primary insomnia. This is false. CBT-I has been shown to be effective in patients with insomnia comorbid to a number of psychiatric and medical conditions. In fact, there is growing recognition that insomnia is itself a syndrome rather than “just a symptom.” This is reflected in the most recent versions of the International Classification of Sleep Disorders (ICSD-3) and Diagnostic and Statistical Manual (DSM-5) which no longer recognize a distinction between primary and secondary insomnia. Persistent insomnia often needs treatment even if the underlying cause is reversed.
Is online CBT-I an evidence-based intervention?
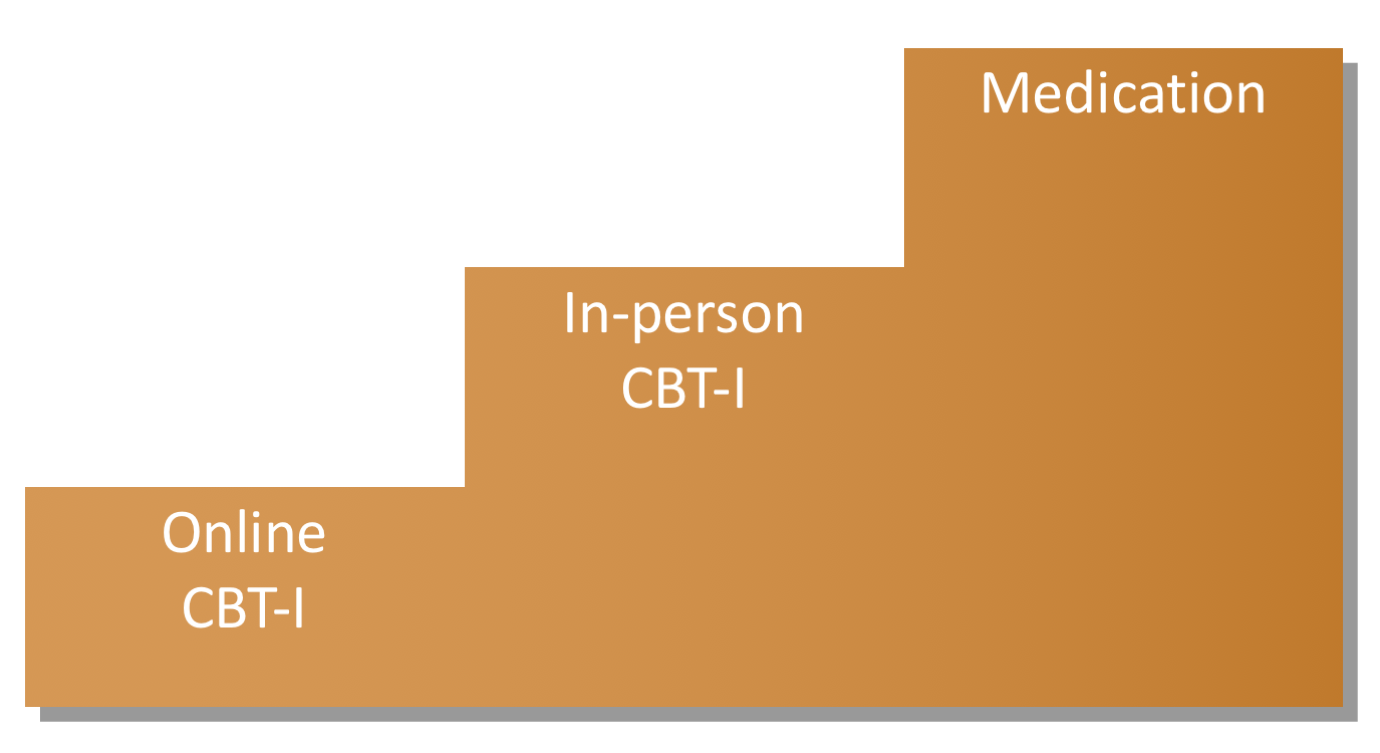
Online CBT-I is a clinically proven intervention which has been tested in many randomized controlled trials. To my knowledge, it is the most well-validated of all online, automated, psychotherapy interventions.
There are at least two reasons why online CBT-I is effective. First, the core techniques of CBT-I are concrete and mechanical. Individual adjustments are baked into the protocols, making it an ideal self-directed intervention.
Second, in-person CBT-I has a large effect size. This helps improve efficacy even when diluted by the lack of nuance, connection, and motivation that an in-person therapist often provides. For a highly motivated participant, the gap between online and in-person CBT-I may be very small.
Given the efficacy and cost-effectiveness of online CBT-I, I recommend treatment using a stepped model of care. If participants don’t respond to Slumber Camp, I strongly encourage a trial of in-person CBT-I to consider alternative diagnoses, troubleshoot problems, and enhance adherence.
Which insomnia subtypes respond to CBT-I?
The current edition of the International Classification of Sleep Disorders (ICSD-3) recognizes three subtypes of insomnia:
| Insomnia subtypes |
| Short-term insomnia disorder (< 3 months) |
| Chronic insomnia disorder (≥ 3 months) |
| Other insomnia disorder (insomnia which does not meet full diagnostic criteria) |
CBT-I’s evidence is primarily derived from patients with chronic insomnia. However, there is good reason to believe that it would be effective in patients with short-term or other insomnia disorder.
CBT-I also has strong evidence in patients with many different medical and psychiatric comorbidities. Although you should always treat underlying disorders to the best of your ability, the distinction between primary and secondary insomnia is not a good reason to withhold CBT-I or pharmacological treatment.
Contraindications
CBT-I is generally well tolerated, and in general, people usually report fewer adverse events from CBT-I than from sedatives and hypnotics. I strongly recommend that patients be especially cautious when driving or operating heavy machinery during the early stages of sleep restriction. In addition, there are several populations where classical sleep restriction—and hence CBT-I—may be inappropriate. These include patients with:
- Untreated sleep apnea
- Bipolar disorder
- Seizure disorders
- Severe parasomnias
These patients may benefit from in-person sessions that take a more gradual approach to foundational CBT-I skills. However, you should consider the risk of decompensation during a temporary period of poor sleep before recommending that any patient engage in CBT-I.
Sleep medications and CBT-I
There is mixed data on whether sleep medications should be continued or tapered during a course of CBT-I. I chose to take a hands-off approach. On Day 27, I ask participants who wish to discontinue chronic medications to discuss a slow, monitored medication taper with their prescribing clinician. I provide the table below to illustrate a potential taper schedule that may be helpful for preventing rebound insomnia and life-threatening benzodiazepine withdrawal syndromes. Patients with long-term treatment or higher doses may need a much longer, slower taper. Please use your clinical judgment when planning a medication taper with your patient.
| Medications commonly prescribed for sleep* | |
| Benzodiazepines (Generic) | Common dose (Weekly taper) |
| Klonopin (Clonazepam) | 0.25-2 mg (0.25 mg) |
| Ativan (Lorazepam) | 0.5-2 mg (0.5 mg) |
| Xanax (Alprazolam) | 0.5-2 mg (0.5 mg) |
| Valium (Diazepam) | 5-10 mg (2.5 mg) |
| Librium (Chlordiazepoxide) | 25-50 mg (12.5 mg) |
| Restoril (Temazepam) | 15-30 mg (7.5 mg) |
| Benzodiazepine-receptor agonists (Generic) | Common dose (Weekly taper) |
| Ambien (Zolpidem) | 5-20 mg (5 mg) |
| Lunesta (Eszopiclone) | 1-3 mg (1 mg) |
| Sonata (Zaleplon) | 5-20 mg (5 mg) |
| Melatonin-receptor agonists (Generic) | Common dose (Weekly taper) |
| Melatonin | 0.5-6 mg (3 mg) |
| Rozerem (Ramelteon) | 8 mg (8 mg) |
| Antihistamines (Generic) | Common dose (Weekly taper) |
| Benadryl (Diphenhydramine) | 25-50 mg (25 mg) |
| Unisom (Doxylamine) | 25 mg (25 mg) |
| Vistaril (Hydroxyzine) | 25-100 mg (25 mg) |
| Antidepressants (Generic) | Common dose (Weekly taper) |
| Oleptro (Trazodone) | 25-200 mg (25 mg) |
| Elavil (Amitriptyline) | 25-100 mg (25 mg) |
| Remeron (Mirtazapine) | 7.5-45 mg (15 mg) |
| Antipsychotics (Generic) | Common dose (Weekly taper) |
| Seroquel (Quetiapine) | 12.5-100 mg (25 mg) |
| Zyprexa (Olanzapine) | 2.5-10 mg (2.5 mg) |
Price and scholarships
My mission is to make scientifically-supported, self-guided insomnia treatment available to everyone who needs it. Slumber Camp is just $29, and need-based scholarships are available to everyone. The application is a single question, as displayed below:
Example Scholarship Application
I am able to pay for Slumber Camp. (That’s the whole application!)
Who are you and what do you think you’re doing?
My name is Jeff Clark, and I’m a board certified psychiatrist. I created Slumber Camp during my residency at the University of Washington because I couldn’t find an affordable, sustainable, and engaging CBT-I program for my patients. I hope that the people you serve find it helpful!
Create a free clinician account
Clinician accounts are completely free. You are welcome to assist patients as they work through Slumber Camp, and you may share excerpts and worksheets in your clinical work so long as you reference SlumberCamp.co. By signing up for a clinician account, you agree to be bound by the terms of our Legal Agreement.
There are two significant differences between participant and clinician accounts. First, participant accounts promote systematic behavioral change by “dripping” lessons out one day at a time, while clinician accounts have immediate access to all of the course material. If you are a clinician who also suffers from insomnia, I recommend that you take full advantage of Slumber Camp by joining as a participant. You’ll only be 28-days behind (and you’ll have actually read all the lessons.)
Second, participant accounts only require one piece of personally identifiable information: an email address. If you choose to create a clinician account, I ask that you please provide basic information about yourself that will allow me to confirm your status as a clinician. (I recognize that not everyone has a public, online presence, and so I may email you and ask for a resume or CV if you leave the website field blank). I try to approve accounts as quickly as possible, but please allow 5-10 business days for approval.
Email (this will also serve as your login):
Name:
Profession/Credential:
Website (or a public clinician profile such as a Doximity, LinkedIn, Psychology Today, or Twitter page):
Password:
Confirm Password:
 |
I certify that I am a clinician. (Not a clinician? Click here to join Slumber Camp.) |
Copyright 2017 - , Wonderberry LLC (dba Slumber Camp).
Slumber Camp teaches the principles of cognitive behavioral therapy for insomnia (CBT-I), an evidence-based therapy. It is not intended to replace the diagnosis, advice, and treatment provided by a qualified healthcare professional. Slumber Camp is not for everyone, and you should talk with your doctor to consider your individual situation before making any health-related decisions. Slumber Camp cannot be held responsible for any harm caused by your choice to engage in this course. By using this website, you agree to be bound by the terms of our Legal Agreement.